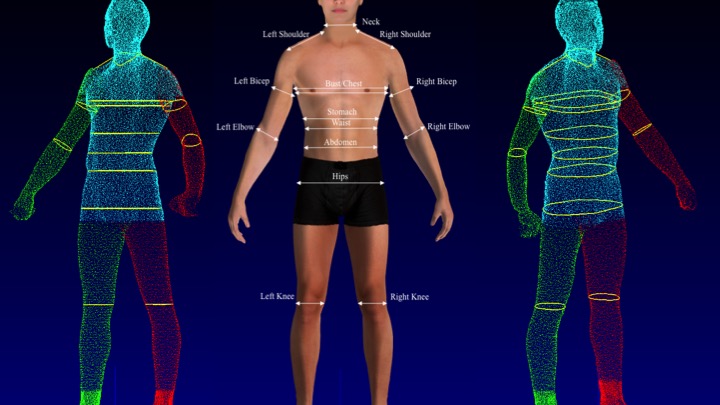
This intriguing topic served as my Master's Thesis. The ultimate goal of this research study is to offer a reference guide for the design of new hospital patient gown (HPG) by determining fit areas of concern and gauging acceptable ranges of size measurements for the HPGs that can be worn by men and women without excessively compromising the patients’ comfort and dignity. Specifically, the study focused on an independent predictor, namely gender, because it offers the most distinctive anthropometric body dimensions between the subgroups. The study adopted multi-dimensional fit and comfort evaluation protocol, among which was the use of a three-dimensional (3D) body scanning technology to measure anthropometric body dimensions of study participants and determine the garment fit problems of the HPG. This study collected subjective fit evaluation through surveys (quantitative), scenarios activities (quantitative), interviews (qualitative), and anthropometric fit assessment through 3D body scanning (quantitative). Based on the characterizations of mixed-methods research proposed by scholars, the study presented quantitative-dominant mixed methods research with between-methods data/methodological triangulation.
The hospital patient gown (HPG), also known as “one-size-fits-all” patient apparel, is the rare design case. In modern society, this garment is worn by almost everyone at least once in their lifetime, and most likely multiple times. Diverse physical profiles of patients, along with their clinical needs, present a unique design challenge to satisfy HPG users with one universal design and one universal size. While medical technology and facilities continually undergo revolutionary innovation, the standard hospital-issued gown has remained essentially unchanged since it was originally designed in the 1920s (Samson, Welsh, & Lamar, 2008). The 21st century users of the HPG are diverse in terms of age, gender, physical profiles and clinical needs, and the outdated design does not successfully meet the needs of patients and healthcare providers alike. For example, a high level of discomfort has been reported by many users of the conventional gown, due to its lack of fit (Park, Sarkar, & Cozza, 2012). In addition, a general misconception that patients are isolated from social interaction has led to a serious disregard of patients’ dignity for the expressive functions of the gown (Cho, 2006). Patients are all too familiar with the embarrassment of trying to hold together flimsy hanging pieces of fabric to avoid exposing their uncovered backsides while walking down a hospital corridor (Park, 2014).
Although some previous attention has been given to redesigning the conventional HPG, the products of these attempts have not yet been widely adopted by hospitals. This is because a satisfying alternative design has not been created based on the comprehension of the hospital’s and the patient’s needs for a new HPG. In any human-centered design process, a comprehensive understanding of the user’s needs and desires offers a critical component for the success of the final design outcomes; because it leads to more effective, efficient, and safer products that likely evoke user satisfaction (Norman, 2013).
Statistical analyses were performed using the IBM SPSS ver. 24.0 software package. To test the normality of data, we conducted Shapiro-Wilk tests at the 95% confidence level and nonparametric Mann-Whitney U tests. Additionally, Pearson correlation and univariate linear regression analyses were performed to understand relationships between continuous variables. Principal component analysis (PCA) were also performed to reduce the dimensionality of variables when appropriate. Descriptive analyses calculated means, standard deviations, frequency and percentage. Additionally, we transcribed qualitative interview data verbatim and analyzed the data using the constant comparison approach (Corbin & Strauss, 2008).